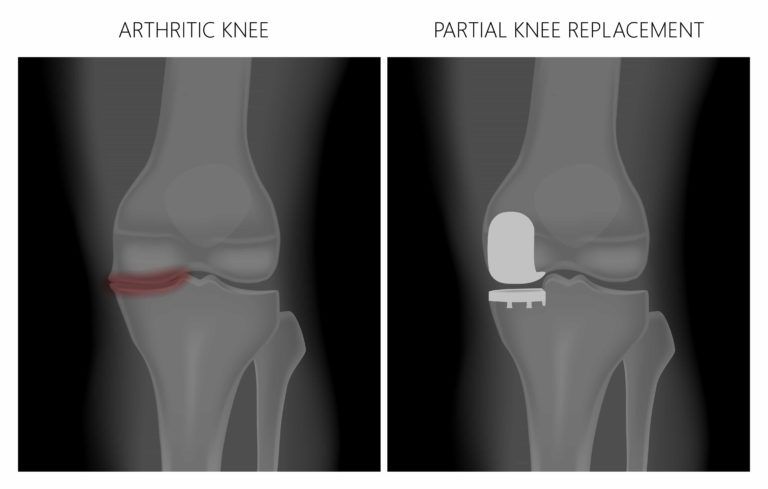
Orthopedic surgeons often perform knee replacements for patients who are limited by diseases and conditions like osteoarthritis or joint injury. But not all patients require a total replacement. Instead, a partial knee replacement can be used to replace only targeted bones and tissues while preserving as much of the natural joint as possible. Most patients pursue partial knee replacements with the goal of eliminating discomfort and returning to an active, pain-free lifestyle.
The knee joint is viewed in three compartments – medial compartment, lateral compartment, and patellofemoral compartment. Patients with arthritis isolated to one of these compartments may be candidates for partial knee replacement surgery. The advantage of partial knee replacement is that the majority of the native joint including the primary ligamentous stabilizers – anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) – are maintained during the procedure. This allows patients to return to sport and activity with the proprioceptive feedback and sensation that they have not had any replacement procedures. Patient’s undergoing partial knee replacements experience less pain, less surgical boneless, and recover faster from surgery. Partial knee replacements, when performed in the correct patients, have high rates of success as compared to other joint replacement procedures. However, if performed in patients with arthritis in more than one compartment they may be at risk for early failure, continued pain, and the possibility of the revision procedure. The goal with each of these operations is to provide the patients with pain-free function of their knee and assurance that they will not require for any subsequent or revision procedures.
Did you know…
that partial knee replacements offer many benefits over total knee replacement procedures? Not only do partial replacements require less invasive surgery, but they also result in less blood loss during surgery on average. Many partial knee replacement patients also experience a shorter recovery period and less post-procedural pain than total knee replacement patients do.
Frequently Asked Questions
Am I a candidate for a partial knee replacement?
You may be a candidate for a partial knee replacement if you are suffering with a knee injury or degenerative disease that is confined to only a single compartment of the knee. Your orthopedist will want to ensure that there are no other, more conservative treatments available before proceeding with a partial knee replacement. To find out if this procedure is right for you, contact your orthopedist to schedule a consultation.
What should I expect during a partial knee replacement?
The partial knee replacement procedure is performed in an inpatient setting with most patients under general anesthesia. An incision is made over the knee, and the diseased or damaged bone and tissue removed from the joint. The new partial prosthetic replaces those areas, and the incision is closed. Most partial knee replacements take less than 1 to 2 hours to complete though patients generally spend an addition 1 to 2 hours in a recovery room.
Will I need to follow any special instructions following my partial knee replacement surgery?
Patients usually remain in the hospital for at least 2 days after a partial knee replacement. During this time, your orthopedists and the hospital medical staff will oversee your recovery to ensure you are not experiencing any complications. Most partial knee replacements take several weeks to heal, during which time your orthopedist may prescribe joint rehab or physical therapy. However, you can expect to be pain-free with restored joint mobility at the end of your rehabilitation and recovery period.
How long is the operation?
The operation is approximately 2 hours.
Can the robotic or computer assistance be used on my knee replacement?
Yes, it can. The use of robotic or computer assistance adds an additional level of accuracy and precision to the procedure to ensure appropriate positioning of components and minimize soft tissue injury.
What are the components made of?
Knee replacements consist of a few different parts. The femoral component is made of cobalt chrome, the tibial component is made of titanium and the insert is composed of highly cross-linked polyethylene. The patellar is resurfaced with a button made of highly cross-linked polyethylene also.
Will I have to get my knee replaced again once it “wears out?”
We have been able to make significant improvements in the components that we use during knee replacement surgery. Combining the newer materials with robotic assistance translates into better outcomes and increased longevity of implants.
How long should I use pain medication?
This is different for each patient; some are able to use Tylenol or Advil after you leave the hospital, and others require pain medication as needed for 2-3 weeks. A general rule is that you should try to decrease your use of these medications as time passes.
How long will I be at the hospital?
Most patients stay in the hospital one night and are discharged the day after their operation. Each patient must meet medical criteria for discharge as well as clear physical therapy. If you require more therapy or medical management we will delay discharge until those needs are addressed.
When should I go to outpatient therapy?
I like to see you in follow up before you go as an outpatient; that way I can tailor your PT to what you need. However, if you feel that it is essential that you begin outpatient PT right away, you can call my office and we will provide a prescription and a list of places.
When can I shower?
Dr. Bawa uses a special waterproof dressing on all incisions to ensure that the surgical site remains clean and dry preventing bacterial infection. After the dressing is removed at one week you can shower normally with the incision exposed. Be sure to pat the skin over the incision dry and avoid rubbing it with a towel. Do NOT soak the incision in a bathtub or Jacuzzi for 6 weeks after surgery.
When can I drive?
You should not drive as long as you are taking narcotic pain medication. Since you are able to sit in regular chairs when you are comfortable, you will be able to drive when you are comfortable sitting and able to lift your leg from side to side. If it is your left knee, you can resume driving when you feel your reaction times are back to normal (about 2-3 weeks). If it is your right knee, you may need to wait another 2 weeks.
I feel “clicking” inside the knee, is this normal?
The clicking is a result of the soft tissues moving across around the knee, or the artificial parts coming into contact with one another. This sensation usually diminishes as your muscles get stronger.
I am experiencing a lot of swelling, is this normal?
Fluid can accumulate in the legs due to the effect of gravity. It is not unusual that you didn’t have it in the hospital, but it got worse when you went home (because you are doing more!) To combat this, you should elevate your legs at night by lying on your back and placing pillows under the legs so that they are above your heart. There are also TEDS stocking (the white stockings from the hospital) that you can put on during the day – have someone help you on with them in the morning, use them during the day, and then take them off at night. If you did not get the TEDS from the hospital, you can purchase knee high, medium (15-20 mm Hg) compression surgical stockings at most drug stores.
Can I work out in the gym?
You can go to the gym and resume upper body workouts (you should be sitting, not standing, when using weights). Do not swim or do any activities involving submerging the incision in water.
When can I return to work?
It depends on your occupation. It is never a mistake to take more time off in the beginning of your recovery, as it will give you time to focus on your knee. I recommend taking at least 4 weeks off after a TKR. Keep in mind that you will still need to use a chair cushion and a high toilet seat for 6 weeks after surgery.
When can I go to the dentist?
Please wait until 3 months after surgery, as the knee is still healing and there is increased blood flow to this area. Please keep in mind that you will need to take antibiotics prior to any dental procedure for at least 2 years after your TKR.
After I have my knee replacement, will I have to take antibiotics before any dental work?
Yes, all dental work which will cause the gums to bleed will require that you take antibiotics before the procedure to prevent bacteria from the mouth and gums from traveling to the artificial joint. This includes routine dental cleaning. Most dentists and oral surgeons are aware of the appropriate treatment so it is important that you inform them that you have an artificial joint. Routine colds and flu, as well as cuts and bruises, do not need to be treated with antibiotics.
Dr. Bawa recommends that patients follow the American Heart Association Standards. Patients should take Amoxicillin 2 grams (4 – 500mg capsules) 1 hour before the procedure. If you are unable to take Amoxicillin, use Clindamycin 600 mg one hour before the procedure for life time.
Can I travel?
In general, I like to see you before you fly within 6 weeks of surgery. If you are traveling by car, you should be sure to take frequent breaks so that you don’t feel too stiff when getting up. On an airplane, I like you to wear compression stockings (if within 1-month postop), and take a couple of walks during the flight. Having an aisle and bulkhead seat will help you get more space.